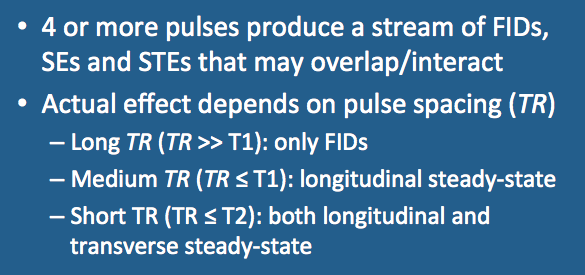
You get some very, very interesting phenomena, especially when the time between pulses (TR) gets shorter and shorter!
To understand what happens we begin by considering the evolution of longitudinal and transverse magnetization during application of a set of evenly spaced RF-pulses as TR is made progressively shorter. Here we assume there is no exogenous spoiling/disruption of the signal by imaging gradients.
To understand what happens we begin by considering the evolution of longitudinal and transverse magnetization during application of a set of evenly spaced RF-pulses as TR is made progressively shorter. Here we assume there is no exogenous spoiling/disruption of the signal by imaging gradients.
Scenario 1. Pulse train with long TR
|
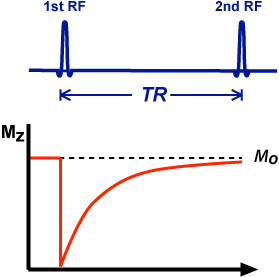
Recall that before any RF-pulses are applied, the spin system reaches a state of thermal equilibrium with its environment. As described in a prior Q&A, a system at equilibrium develops a net longitudinal magnetization (Mz) whose initial maximum value is denoted Mo.
Each RF-pulse rotates some (or all) of Mz into the transverse plane. During the TR interval, Mz will regrow in an exponential fashion with time constant T1. If TR is sufficiently long (the usual requirement is TR > 4-5x T1), Mz will have time to completely recover and be restored to its full initial magnetization Mo. |
|
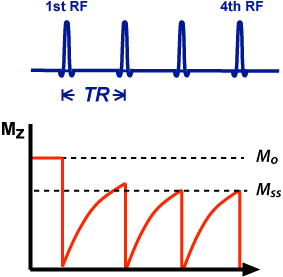
Scenario 2. Pulse train with medium TR
In this scenario, TR is now the same or shorter than T1. Here the second and subsequent pulses occur before Mz has returned to its initial value (Mo). After a few pulses a new steady-state longitudinal magnetization (Mss) will be established, where Mss < Mo. This phenomenon is called partial saturation, meaning that the spin system has not fully relaxed back to its equilibrium condition. So now we know what's happening with Mz, but what about the transverse magnetization (Mxy) and the MR signals? As shown in the diagram, each RF-pulse generates a free induction decay (FID). Every pair of RF-pulses generates a spin echo (SE), and every triad of pulses generates a stimulated echo (STE). Because the pulses are evenly spaced, the SE's and STE's occur at the same time coming to maximum values just before the next RF-pulse. |
|
Scenario 3. Pulse train with short TR
If TR is made even shorter (≤T2*) the FID following each RF-pulse does not completely die out before the SE/STE component begins to form. The tails of the FIDs and SE/STEs merge together. In this situation the transverse signal never completely disappears and the result is called a steady state free precession (SSFP).
|
Similar to the graphs above for the longitudinal magnetization (Mz), the diagram below shows what happens to the transverse magnetization (Mxy) as TR is progressively reduced to the order of T2 or less.
The combined use of gradients and phase changes of these RF-pulses will significantly affect whether M'ss is even allowed to exist, and if so, and exactly how it will form. This leads to two basic categories of GRE sequences discussed in detail in several later Q&As.
- Spoiled-GRE sequences: M'ss is disrupted/prevented from forming.
- Coherent-GRE sequences: M'ss is nutured/preserved.
Advanced Discussion (show/hide)»
Additional Notes on Transverse Steady State
There are several additional conditions for the formation of a transverse steady state, also known as steady-state free precession, which (for simplicity of explanation) were not included in the discussion above. These include:
References
Carr HY. Steady-state free precession in nuclear magnetic resonance. Phys Rev 1958; 112:1693-1701. (Another paper with heavy math and physics, but one serious MR students should have in their libraries).
Chavhan GB, Babyn PS, Jankharia BG et al. Steady-state MR imaging sequences: physics, classification, and clinical applications. Radiographics 2008;28:1147-1160.
Elster AD. Gradient echo imaging: techniques and acronyms. Radiology 1993; 186:1-8.
Gyngell ML. The steady-state signals in short-repetition-time sequences. J Mag Reson 1989;81:474-483.
Carr HY. Steady-state free precession in nuclear magnetic resonance. Phys Rev 1958; 112:1693-1701. (Another paper with heavy math and physics, but one serious MR students should have in their libraries).
Chavhan GB, Babyn PS, Jankharia BG et al. Steady-state MR imaging sequences: physics, classification, and clinical applications. Radiographics 2008;28:1147-1160.
Elster AD. Gradient echo imaging: techniques and acronyms. Radiology 1993; 186:1-8.
Gyngell ML. The steady-state signals in short-repetition-time sequences. J Mag Reson 1989;81:474-483.
Related Questions
What is a stimulated echo?
What is a stimulated echo?